Utility of Brain SPECT for Traumatic Brain Injuries
Traumatic brain injury (TBI), also known as concussion, is a highly debilitating injury that affects a large population every year. Simply put, TBI is a change in brain function as a result of external forces. There are a wide-variety of symptoms that can manifest as a result of TBI. These symptoms include chronic headaches, fatigue, and depression, just to name a few.
Traditionally, clinicians have relied on computed tomography (CT), Magnetic Resonance Imaging (MRI), electroencephalograms (EEGs), neuropsychological evaluations, Diffuse Tensor Imaging (DTI), Videonystagmography (VNG), etc. when diagnosing brain abnormalities in those who have sustained TBI. However, in many patients who complain of post-concussive symptoms, these traditional imaging techniques may be unable to detect neurological abnormalities. This can lead to controversy as to the origin of the post-concussive symptoms. Without objective proof of cerebral dysfunction, clinicians rely more on the history of the injury in order to make the diagnosis of TBI. The more recent advent of the single-photon emission computerized tomography (SPECT) scan helps in the objective diagnosis of TBI, as research has shown it to be a reliable detector of organic brain dysfunction among patients who have experienced TBI and complain of post-concussive symptoms.
How is SPECT Performed?
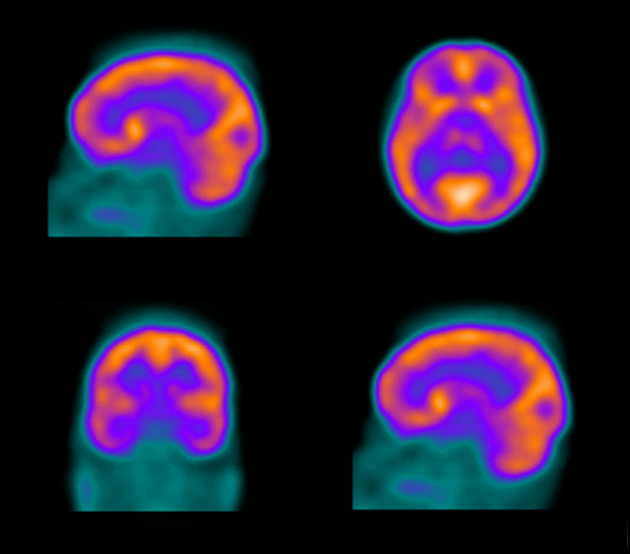
SPECT is a nuclear imaging test that is used to analyze the function of internal organs. Before the SPECT scan is performed patients are injected intravenously with a radioactive tracer substance. The tracer that is injected emits gamma rays and is able to cross the blood-brain-barrier. After receiving the tracer injection, patients typically wait for some period of time before the SPECT scan is performed in order to allow the tracer to reach the organ of interest. After this time has elapsed the patient will lay flat on a table. The SPECT scanner is a circular device that rotates around the patient. Attached to the device is a camera that detects the gamma rays emitted from the radioactive tracers. SPECT scans develop three dimensional images that can be used to analyze the function of internal organs. In the brain, SPECT is used to detect cerebral perfusion. Levels of cerebral perfusion may be an accurate representation of neurological condition as research has shown that cerebral blood flow is closely linked to neuronal activity.
Changes in SPECT following Traumatic Brain Injury
SPECT may be used to detect functional damage from TBI that cannot be seen on other more traditional brain scans such as CT and MRI. When brain areas have been damaged as a result of TBI, SPECT scans normally show marked areas of decreased cerebral activity. In some cases cerebral hyperactivity has been observed over brain areas impacted by TBI. Research has shown that the severity of perfusion abnormality observed in SPECT scans may be correlated with the severity of TBI.
In several studies SPECT scans show perfusion deficits in similar areas of the brain after TBI. The areas of the brain that most frequently show perfusion deficits after TBI are the temporal and frontal lobes and the parieto-occipital-temporal junction. Studies have also noted that the regions of hypo-perfusion observed from SPECT are not necessarily correlated with the site that the brain was impacted from the TBI.
SPECT as a diagnostic tool for treating traumatic brain injury
SPECT may be a reliable tool in determining whether TBI will lead to post-concussive symptoms. A SPECT scan that shows normal cerebral perfusion after a patient sustains a TBI could be an indicator of better prognosis. SPECT scans that show abnormal cerebral perfusion after TBI frequently are not able to reliably predict the severity of chronic TBI symptoms and require follow up SPECT scans three months after the initial scan.
When SPECT is repeated three months after the injury, patients who report post-concussive symptoms frequently show abnormal cerebral perfusion. The implications of this finding are significant. Historically, when patients would report post-concussive symptoms deficits in brain function that could be used to explain these symptoms were often unable to be detected by CT and MRI scans. This is a diagnostic impediment because without the observation of neurological deficits it may be difficult to distinguish whether post-concussive symptoms stem from brain damage or from psychological side-effects of the traumatic accident or a combination of both. Research has shown that SPECT may be able to consistently provide objective proof of organic dysfunction among TBI survivors that complain of post-concussive disturbances. If this is the case, SPECT has the potential to be a critical clinical tool when treating and diagnosing post-concussive symptoms.
Our Doctors
Life Care Planners

Physical Medicine & Rehabilitation, Pain Medicine, Brain Injury Medicine
Dr. Miranda-Grajales
YEARS years of experience



Master of Divinity, Specializing in Neuropsychology
Dr. Brandi Buchanan
YEARS years of experience